In the battle against obesity, laparoscopic adjustable gastric banding, commonly known as Lap-Band surgery or gastric band surgery has emerged as a viable solution for individuals struggling to achieve significant and sustainable weight loss through traditional methods. This minimally invasive bariatric procedure offers an effective means of reducing stomach capacity, promoting early satiety, and facilitating long-term weight management for individuals with obesity or obesity-related health conditions. In this comprehensive guide, we’ll explore the intricacies of Lap-Band surgery, including its procedure, benefits, risks, candidacy criteria, recovery process, and post-operative lifestyle changes.
Understanding Lap-Band Surgery
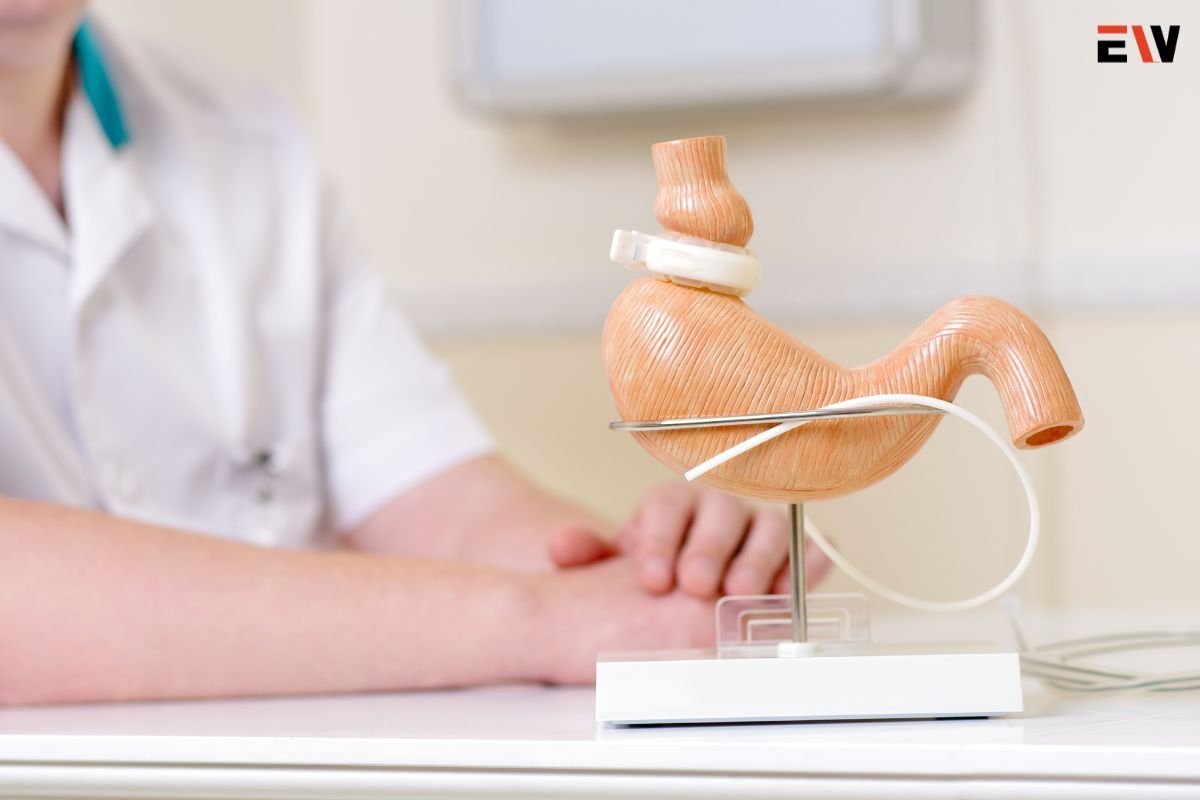
Lap-band surgery is a type of bariatric surgery that involves the placement of an adjustable silicone band around the upper part of the stomach, creating a smaller stomach pouch and restricting food intake. This restrictive procedure helps individuals feel full more quickly, leading to reduced calorie consumption and gradual weight loss over time.
The Lap-Band Procedure
During gastric band surgery, a surgeon makes small incisions in the abdomen and inserts a laparoscopic camera and surgical instruments to access the stomach. The adjustable silicone band is then placed around the upper portion of the stomach, forming a small pouch. The band is connected to an access port implanted beneath the skin, allowing the surgeon to adjust the band’s tightness by injecting or removing saline solution.
Benefits of gastric band surgery
1. Effective Weight Loss:

Lap-band surgery can lead to significant and sustained weight loss, with many patients achieving a loss of 50% or more of their excess body weight within the first few years after surgery.
2. Reversible and Adjustable:
Unlike some other bariatric procedures, gastric band surgery is reversible and adjustable, allowing for modifications to the band’s tightness or removal of the band if necessary.
3. Minimally Invasive:
Lap-band surgery is performed laparoscopically, resulting in smaller incisions, reduced post-operative pain, shorter hospital stays, and quicker recovery times compared to open surgery.
4. Low Risk of Nutritional Deficiencies:
Because gastric band surgery does not involve rerouting or bypassing the digestive tract, the risk of nutritional deficiencies is lower compared to procedures like gastric bypass surgery.
Risks and Complications
1. Band Slippage or Erosion:
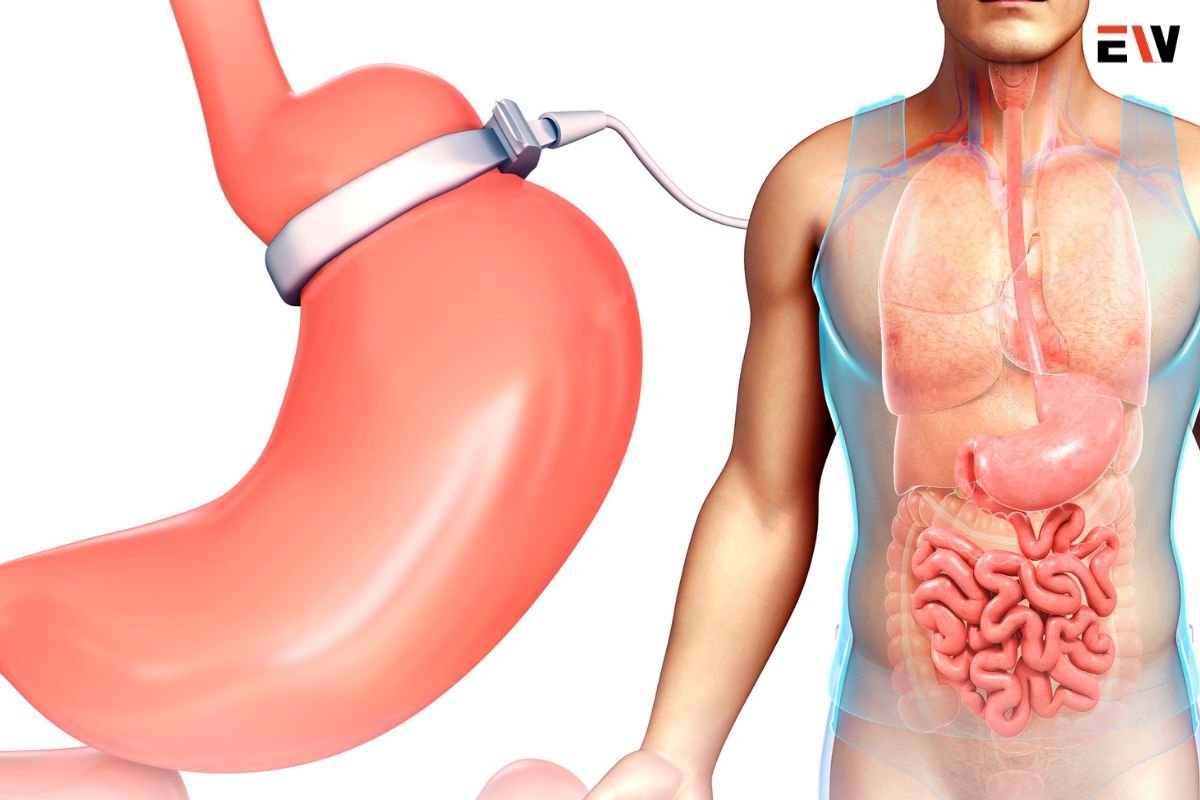
In some cases, the lap band may slip out of position or erode into the stomach tissue, requiring surgical intervention to reposition or remove the band.
2. Gastrointestinal Symptoms:
Patients may experience nausea, vomiting, reflux, or difficulty swallowing, especially if the band is too tight or improperly positioned.
3. Band Adjustment Issues:
Achieving optimal band tightness may require multiple adjustments over time, and some patients may struggle to find the right balance between restriction and comfort.
4. Long-Term Weight Loss Maintenance:
While Lap-Band surgery can facilitate initial weight loss, long-term success depends on adherence to dietary and lifestyle changes, and some patients may experience weight regain over time.
Candidacy Criteria
Candidates for gastric band surgery typically meet the following criteria:
- Body mass index (BMI) of 40 or higher, or BMI of 35 or higher with obesity-related health conditions such as type 2 diabetes, hypertension, or sleep apnea.
- Unsuccessful attempts at weight loss through diet, exercise, and other non-surgical interventions.
- Commitment to lifelong dietary and lifestyle changes is necessary for successful weight loss and maintenance.
Recovery Process
After gastric band surgery, patients typically experience a gradual recovery process, including:

- A liquid or pureed diet for the first few weeks, followed by a gradual transition to solid foods.
- Regular follow-up appointments with the surgeon to monitor weight loss progress, adjust the band tightness as needed, and address any concerns or complications.
- Incorporation of regular physical activity and behavior modifications to support long-term weight loss and maintenance.
Post-Operative Lifestyle Changes
To maximize the benefits of Lap-Band surgery and promote long-term weight loss success, patients are encouraged to:
- Adopt a nutritious, balanced diet focused on lean protein, fruits, vegetables, and whole grains.
- Practice mindful eating habits, including chewing food thoroughly, eating slowly, and stopping when satisfied.
- Stay physically active by engaging in regular exercise, such as walking, swimming, or strength training, to support weight loss and overall health.
- Attend support groups or counseling sessions to address emotional, psychological, and behavioral factors that may influence eating behaviors and weight management.
Conclusion
Lap-band surgery offers a safe, effective, and reversible option for individuals seeking significant weight loss and improved health outcomes. By understanding the procedure, benefits, risks, candidacy criteria, recovery process, and post-operative lifestyle changes associated with gastric band surgery, patients can make informed decisions and embark on a transformative journey toward a healthier, happier life. As part of a comprehensive approach to obesity management, gastric band surgery has the potential to empower individuals to achieve their weight loss goals and reclaim their health and vitality.